Medical Research Funding: Impacts on Patient Safety
Medical research funding plays a crucial role in advancing healthcare and ensuring patients’ rights and safety within clinical studies. Without proper financial backing, institutions struggle to maintain compliance with necessary oversight practices, like those enforced by Institutional Review Boards (IRBs). The impact of NIH funding cannot be overstated, as it directly supports these essential oversight structures, which uphold clinical research safety and protect patient rights. Unfortunately, recent funding cuts threaten to disrupt critical studies, putting vulnerable populations at risk and jeopardizing the integrity of the research process. In an environment where patient trust is paramount, the adverse effects of funding shortfalls are felt deeply in the medical community.
The financial resources allocated for medical research are essential for promoting innovation and upholding ethical standards in clinical trials. The cessation of grants and federal support undermines vital mechanisms, such as institutional oversight by IRBs, which are designed to safeguard patient welfare. When research initiatives are financially compromised, the ramifications stretch far beyond economics, affecting the safety and rights of research participants. Additionally, as financial backing dwindles, collaborative projects can suffer delays and complications, further isolating healthcare advancements. This nexus between funding and research efficacy highlights the indispensable nature of sustained support for the longevity and success of medical research.
Impact of NIH Funding on Patient Safety in Research
National Institutes of Health (NIH) funding plays a crucial role in safeguarding the rights and safety of patients participating in medical research. This funding is essential for the rigorous Institutional Review Board (IRB) processes that ensure compliance with ethical standards and regulations governing human subjects. An effective IRB must conduct thorough reviews of research proposals, assessing risks and determining informed consent protocols to protect participants from harm. When NIH funding is stable, it enables IRBs to devote necessary resources to supervise studies ethically, effectively contributing to the overall safety net for patients.
However, cuts in NIH funding directly threaten these safety mechanisms. With less financial support, IRBs may lack the capacity to engage in comprehensive reviews of research proposals, leading to potentially dangerous oversights. This situation stresses the importance of adequate funding not just for initiating research but also for the continuous oversight required to protect patient rights. Research that might have high public health implications could falter under such constraints, highlighting the need for robust financial backing in the realm of medical research.
The Role of IRB Oversight in Clinical Research
Institutional Review Boards (IRBs) serve as the backbone of ethical oversight in clinical research. They are responsible for reviewing the methodological aspects of research studies to ensure that patients’ rights are preserved and their welfare prioritized. By implementing strict protocols to assess study designs and informed consent processes, IRBs ensure that the delicate balance between scientific inquiry and ethical responsibility is maintained. This oversight is essential, especially in high-stakes research scenarios where vulnerable populations may be involved.
Moreover, the challenges IRBs face are compounded when funding cuts occur, as fewer resources mean less ability to monitor ongoing research effectively. For example, during periods of financial constraint, IRBs may find it more challenging to hire experienced staff or provide adequate training to new members. This can lead to a dilution of the oversight quality that is critical for ensuring patient safety, thereby highlighting the significance of sustained funding for ethical governance in healthcare.
Consequences of Funding Cuts on Medical Research
The implications of funding cuts are profound and multifaceted within the medical research landscape. Projects that receive federal grants often provide significant insights and innovations, particularly in the fields of oncology or infectious diseases. When substantial funding is withdrawn, such as the recent freeze on $2 billion in federal grants to Harvard, ongoing research projects face abrupt termination or severe delays. The halt of these studies doesn’t just impede scientific progress; it can also threaten the health and safety of individuals participating in these crucial trials.
Ultimately, funding cuts can severely impact public trust in clinical research. As studies encounter funding obstacles and a resulting lack of oversight, participants may grow wary and skeptical of research endeavors. This erosion of trust can have lasting effects, as patients may be less likely to volunteer for future studies, undermining the entire research process. Hence, the call for reliable funding sources is crucial to maintaining not only the ethical standards of research but also ensuring the community’s willingness to engage in clinical trials.
Ensuring Patient Rights Through Research Oversight
Patient rights protection is a fundamental aspect of conducting ethical medical research. Maintaining vigilant oversight through IRBs guarantees that individuals who volunteer for studies are fully informed of the risks and benefits associated with their participation. This protection extends beyond mere consent; it encompasses the continuous obligation to safeguard participants from potential harm and to advocate for their well-being throughout the research process.
Research institutions must place a high priority on the ethical responsibility of protecting patient rights, particularly in light of funding fluctuations. Reduced financial support can lead to inadequate staffing and resources for IRBs, ultimately undermining this crucial aspect of medical research. Therefore, finding sustainable funding solutions is essential for reinforcing patient rights protections and ensuring that ethical standards are consistently met in the face of ongoing challenges.
The Historical Context of IRBs and Medical Ethics
The establishment of Institutional Review Boards (IRBs) was a direct response to historical violations of patient rights in research. Cases like the Tuskegee Syphilis Study revealed the dire need for structured oversight and accountability in clinical trials. Learning from these past mistakes, the IRB system has become an integral component of the research infrastructure, tasked with protecting patients and advancing ethical standards in health studies.
This historical perspective underscores the importance of IRBs in maintaining ethical practices amidst evolving medical protocols. It serves as a reminder of the consequences of neglecting patient welfare in the pursuit of scientific knowledge. Continuous funding is essential not just for operational capacity but also for sustaining the ethical evolution that these boards represent in modern medical research.
Addressing the Challenges of Multi-Site Research
Multi-site research studies present unique challenges that require careful consideration and robust oversight. The NIH’s policy to engage single IRB reviews streamlines the oversight process and reduces redundancy across multiple institutions. This efficiency not only expedites the research timeline but also ensures that patient protections remain consistent irrespective of the study site. The collaboration among hospitals and research organizations facilitated by this policy relies heavily on adequate funding to maintain its efficacy.
Without sufficient resources, this relationship can falter, complicating participation and compliance between institutions. As restrictions tighten due to funding cuts, participating sites may find themselves unable to align on ethical standards or conduct necessary oversight efficiently. Therefore, ensuring consistent funding for multi-site research initiatives is critical to uphold research quality and patient care standards across all participating locations.
The Health and Safety Risks to Participants
The well-being of participants in clinical trials is of paramount importance, yet funding cuts place this very safety at risk. Studies that halt mid-process can lead to unresolved complications for participants who enroll with the expectation of comprehensive evaluation and care. Financial instability impedes the necessary follow-ups and monitoring that are integral to patient safety protocols, potentially exposing them to unknown risks and consequences.
It is essential for research institutions to recognize that funding serves as a lifeline for maintaining health and safety standards. Without sufficient financial support, investigators may be forced to compromise on essential practices, undermining existing protocols and patient protections. Continuous advocacy for medical research funding must emphasize the direct correlation between financial backing and participant safety, stressing the grave implications that cuts can have on human health.
Future Directions for Medical Research Funding
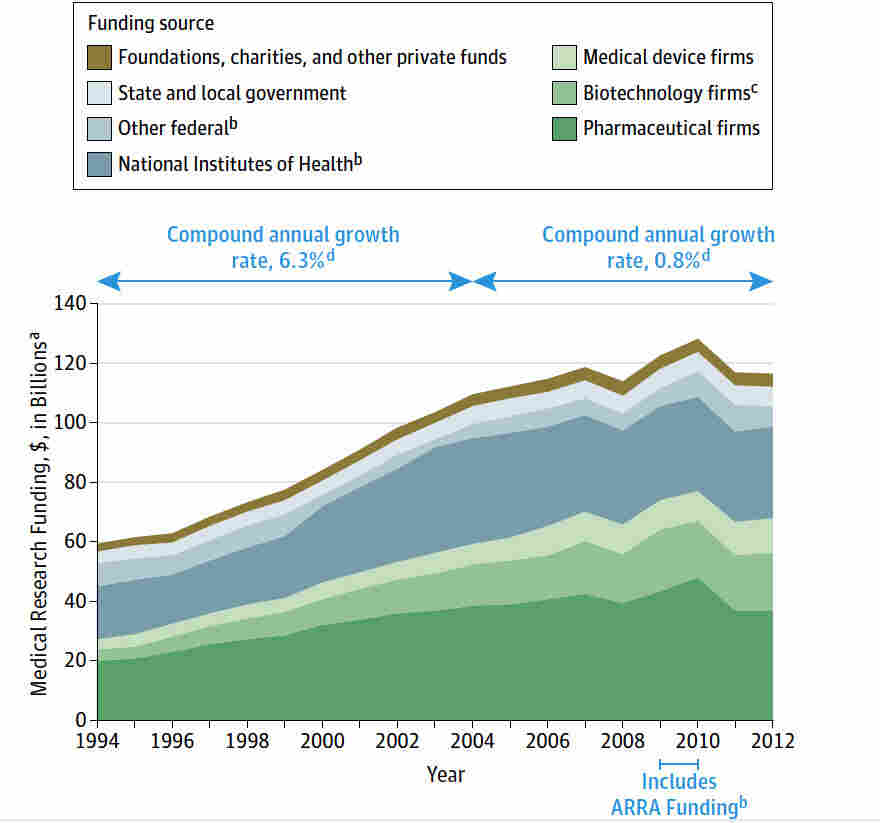
Looking ahead, it is crucial to establish sustainable funding models for medical research that ensure patient rights and safety remain at the forefront of all initiatives. This requires a collaborative approach involving federal funding agencies, private sector donations, and community engagement to create a diversified funding base. Ensuring that research institutions receive reliable financial support will not only improve operational efficiency but also buffer against the detrimental effects of future funding cuts.
In addition, institutional leaders must become advocates for transparent funding policies that prioritize patient welfare in all aspects of clinical research. By fostering a culture of accountability and ethics, the medical research community can work together to follow the legacy of IRBs and ethical oversight systems designed to protect human subjects, ensuring that participants can trust the process and outcomes of their involvement in research.
The Importance of Community Engagement in Research
Community engagement is an increasingly vital component of successful medical research, particularly in enriching the fabric of participant recruitment and retention. When research initiatives actively involve the communities they aim to serve, they foster trust and encourage participation. This engagement is essential not only for improving patient rights but also for ensuring that research findings are directly applicable to the populations most affected by specific health issues.
Moreover, engaging with community stakeholders can provide valuable insights into potential barriers that participants may face, enhancing the IRB’s ability to protect patient rights. To implement meaningful community engagement practices, adequate funding is necessary to support outreach efforts, educational initiatives, and collaborative partnerships. By securing robust financial resources, research institutions can cultivate relationships that translate into improved health outcomes and bolstered societal trust in the research process.
Frequently Asked Questions
How does NIH funding impact the safety and rights of patients in medical research?
NIH funding plays a crucial role in safeguarding the safety and rights of patients involved in medical research. It ensures that all studies are subjected to rigorous oversight by Institutional Review Boards (IRBs), which assess research proposals to protect participant welfare and ensure informed consent. Additionally, NIH grants often cover indirect costs related to IRB oversight, thus enhancing patient protection across various research sites.
What is the role of IRB oversight in medical research funding?
IRB oversight is essential in the context of medical research funding as it ensures that research proposals undergo thorough ethical reviews before approval. This process helps assess risks, ensure patient rights are respected, and monitor ongoing safety throughout the study. Increased federal research funding, such as NIH grants, facilitates robust IRB operations, which are vital for the integrity of clinical trials.
How do funding cuts affect clinical research safety and patient rights?
Funding cuts can severely disrupt clinical research safety and patient rights by limiting the resources available for IRB oversight and participant monitoring. When federal grants, like those from the NIH, are cut, institutions like Harvard may face stop-work orders, preventing new participants from joining studies and halting essential oversight. This can lead to deterioration in research quality and participant trust.
What is the relationship between NIH funding and patient rights protection in clinical studies?
NIH funding directly supports structures and systems that uphold patient rights protection in clinical studies. By financing IRB functions and compliance with ethical regulations, NIH grants ensure that participant welfare is prioritized. The comprehensive review processes mandated by this funding help to reinforce trust in research while safeguarding participants from potential harms.
What are the consequences of halted funding for research initiatives and patient safety?
Halted funding for research initiatives can have severe consequences for patient safety, as it disrupts ongoing studies and limits the ability of IRBs to enforce oversight. This can lead to increased risks for participants, as studies may be paused midstream, affecting not only the research integrity but also public trust in medical research practices.
| Key Points | Details |
|---|---|
| Funding Freeze Impact | The Trump administration’s freeze of over $2 billion in federal research grants to Harvard has disrupted patient safety efforts. |
| SMART IRB Overview | SMART IRB facilitates oversight of multi-site medical research to ensure patient rights and safety. |
| Role of IRBs | IRBs review research proposals to protect participants through informed consent, risk assessment, and safety monitoring. |
| Historical Context | Past medical experiments highlighted the need for ethical oversight and public trust in research. |
| Consequence of Cuts | Funding cuts risk halting studies, causing harm to participants, and reinforcing public skepticism. |
Summary
Medical research funding is crucial for ensuring patient safety and ethics in clinical trials. The recent freeze of federal grants has severe implications for research oversight, ultimately affecting participants and the trajectory of medical advancements. Without sufficient funding, essential systems like the SMART IRB cannot operate effectively, leading to halted studies and diminished public trust in medical research.