TIM-3 therapy for Alzheimer’s disease presents a groundbreaking approach that merges cancer treatment strategies with neurodegenerative challenges. This innovative therapy focuses on inhibiting the checkpoint molecule TIM-3, which plays a critical role in regulating the immune response of microglia in the brain. Research has shown that manipulating TIM-3 can release microglia from their inhibited state, allowing them to effectively target and clear amyloid plaques—hallmarks of Alzheimer’s. By enhancing the immune system’s ability to combat plaque accumulation, TIM-3 therapy opens the door to potential cognitive improvement in Alzheimer’s patients, a significant advancement considering the complex nature of Alzheimer’s treatment. As we explore the intersection of immune system checkpoint modulation and neuroinflammatory processes, TIM-3 therapy stands poised to transform strategies in the ongoing battle against Alzheimer’s disease.
The emerging TIM-3 therapy for Alzheimer’s disease symbolizes an exciting frontier in the management of neurodegenerative disorders. This approach utilizes an immune checkpoint mechanism, typically associated with cancer therapies, to enhance brain health by targeting the hyperactivity of the immune system’s microglial cells. Through the deactivation of the TIM-3 molecule, researchers aim to restore the natural ability of these cells to dismantle plaques that impede cognitive functions in individuals suffering from memory loss conditions. With precision and ambition, this technique not only sheds light on the intricate relationship between the immune system and Alzheimer’s pathology but also signifies a pivotal moment for advancing effective dementia treatments using previously established cancer therapeutics. As investigations continue, the hope for significant cognitive enhancement in Alzheimer’s patients remains at the forefront of this promising research.
The Role of TIM-3 in Alzheimer’s Disease
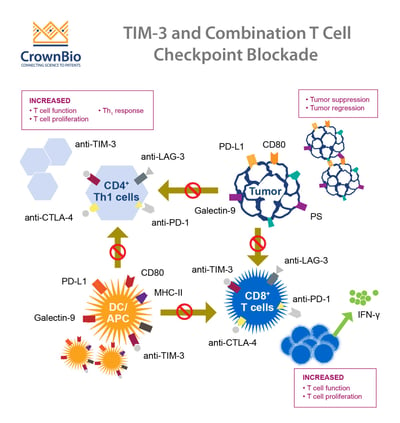
Recent studies have highlighted the significance of the TIM-3 immune checkpoint molecule in the context of Alzheimer’s disease (AD). TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, acts as a brake on the immune response by inhibiting microglia, which are the brain’s primary immune cells. This inhibition can lead to the accumulation of amyloid-beta plaques, a hallmark of Alzheimer’s, as microglia fail to clear these toxic substances. The presence of TIM-3 in microglia is significantly higher in individuals with the genetic polymorphism associated with Alzheimer’s, showcasing its detrimental role in promoting the disease progression by impeding crucial cognitive functions.
Understanding the mechanics of TIM-3 could unlock new avenues for Alzheimer’s treatment strategies. By deleting or inhibiting TIM-3 in experimental models, researchers observed enhanced microglial activity in plaque clearance and cognitive recovery. This suggests that potential therapies targeting TIM-3 could lift the inhibitory signals in the immune response, leading microglia to become more active in clearing plaques and restoring memory functions. As such, TIM-3 therapy has emerged as a promising frontier, where existing cancer treatment methodologies could be repurposed to ameliorate Alzheimer’s symptoms.
The Impact of Immune System Pathways in Alzheimer’s Treatment
The immune system’s checkpoints, like TIM-3, play a crucial role not only in cancer treatment but also in the emerging field of Alzheimer’s treatment. The traditional role of these checkpoints involves preventing autoimmunity by regulating T-cell responses. In the context of Alzheimer’s, the ability of microglia to engulf harmful amyloid plaques is hampered by these checkpoints, overlaying a complex layer of immune system response that researchers are only beginning to understand. The discovery that inhibiting TIM-3 can lead to increased microglial activity offers a dual approach to Alzheimer’s therapy: it not only targets plaque clearance but also seeks to optimize cognitive function through immune modulation.
Moreover, the repurposing of cancer treatment strategies to address Alzheimer’s signals a growing trend in pharmacological research. Immune checkpoint inhibitors successfully employed in oncology are being scrutinized for their potential to enhance microglial function and promote cognitive improvement in Alzheimer’s patients. This shift to re-evaluating existing drugs offers a more immediate pathway to therapeutic options compared to developing entirely new medications, which often face arduous regulatory hurdles.
Microglial Dynamics and Alzheimer’s Pathology
Microglia serve as the brain’s resident immune cells, continuously surveying their environment to maintain homeostasis and respond to pathological threats. In Alzheimer’s disease, these cells undergo a dramatic transformation, contributing to neuroinflammation and further exacerbating the disease. The overexpression of inhibitory checkpoint molecules like TIM-3 can cause microglia to enter a state of functional paralysis, preventing them from effectively clearing amyloid plaques. This dynamic interplay underscores the essential role of microglia in cognitive health and disease progression.
Research indicates that enhancing microglial activation through TIM-3 inhibition could restore their ability to manage synaptic pruning and plaque clearance, leading to significant cognitive improvements in Alzheimer’s models. The potential for therapy hinges on understanding these cellular mechanisms, driving the search for novel treatment pathways that target microglial function to remediate Alzheimer’s pathology. Increasing our comprehension of microglial biology and its interaction with Alzheimer’s will pave the way for breakthroughs in treatment.
Cognitive Improvement in Alzheimer’s: Insights from TIM-3 Studies
The quest for cognitive improvement in Alzheimer’s patients has led researchers to explore innovative therapies targeting molecules like TIM-3. In animal studies, models lacking TIM-3 have shown noticeable enhancements in memory and learning capabilities, despite the presence of amyloid-beta plaques. The reinforcement of synaptic connections and neural pathways via microglial activity, unrestrained by TIM-3, suggests a blueprint for future therapeutic applications that could potentially translate to human subjects. This discovery has far-reaching implications for the standards of care in Alzheimer’s treatment.
Utilizing TIM-3 therapy could not only facilitate the reduction of amyloid plaques but also promote overall brain health and cognitive function. As researchers continue to evaluate the outcomes of TIM-3 inhibition in Alzheimer’s models, there is a growing optimism regarding the development of clinical therapies that could lead to profound cognitive benefits. By leveraging existing knowledge and targeting immune system checkpoints, the fight against Alzheimer’s could take a significant turn towards efficacy and improved quality of life for patients.
Exploring Cancer Treatment Repurposing for Alzheimer’s Therapy
Repurposing established cancer therapies is emerging as a promising strategy in the fight against Alzheimer’s disease. The mechanisms seen in cancer treatments, specifically those targeting immune checkpoints like TIM-3, are being re-examined for their potential applications in Alzheimer’s research. In similar ways to how checkpoint inhibitors release the brakes on T-cells in cancer, they could theoretically rejuvenate microglial activity to improve plaque clearance and cognitive functions. This innovative approach could significantly alter treatment paradigms for neurodegenerative diseases.
Additionally, medical research increasingly emphasizes the benefits of repurposing existing drugs due to their prior safety profiles, dosage guidelines, and regulatory process advantages. By redirecting resources from areas that have seen diminishing returns towards developing TIM-3-targeted therapies for Alzheimer’s, researchers hope to fast-track treatments that can enhance patient outcomes. Bridging cancer treatment with Alzheimer’s therapy highlights parallels that may hasten breakthroughs, fostering a multidisciplinary approach to neurodegenerative disease management.
Potential Future Therapies Utilizing Anti-TIM-3 Antibodies
As research progresses, the focus is turning towards developing potential therapies that employ anti-TIM-3 antibodies specifically designed to counteract the inhibitory effects on microglia. This novel approach aims to deactivate the immune checkpoint mechanism that currently hampers the brain’s ability to clear amyloid plaques, leading to Alzheimer’s progression. Utilizing tailored antibodies could signify a breakthrough in targeting the underlying causes of cognitive decline and memory loss associated with Alzheimer’s.
Moreover, the implementation of anti-TIM-3 antibodies may provide a targeted strategy that mitigates adverse effects seen in broader immune system interventions. By selectively modulating TIM-3 expression, it is conceivable that these therapies could enhance microglial function without the extensive repercussions associated with systemic immune activation. The next era of Alzheimer’s treatment could be shaped by innovations in immunotherapy, allowing for personalized and effective interventions that directly target the neuroinflammatory profiles characteristic of the disease.
Genetic Polymorphisms and Alzheimer’s Disease Risk
The genetic landscape of Alzheimer’s disease reveals a fascinating interplay between specific polymorphisms and the manifestation of the condition. One such polymorphism occurs in the TIM-3 gene, which has been linked to increased risk for late-onset Alzheimer’s. Understanding these genetic factors is crucial, as they not only elucidate the mechanisms behind disease vulnerability but also provide potential biomarkers for early detection and targeted treatment strategies. Identifying individuals with this genetic predisposition may allow for interventions that could prevent or delay the onset of symptoms.
Research into TIM-3 and its associated genetic risk factors underscores the broader significance of genetics in Alzheimer’s cognition. Drilling down into these connections may also reveal tailored therapeutic approaches based on individual genetic profiles, paving the way for precision medicine in tackling Alzheimer’s. As science continues to harness the power of genetics, the potential for custom-designed therapies targeting specific pathways such as TIM-3 becomes more conceivable, fortifying the battle against cognitive decline in a personalized manner.
The Challenge of Amyloid Beta and Vascular Health
A significant challenge in the development of Alzheimer’s therapies revolves around the interaction of amyloid beta with vascular health. Amyloid beta accumulates not only in the brain but also within blood vessels, where it can provoke strokes and other systemic issues that complicate treatment. The dual localization of amyloid beta complicates therapeutic measures, especially those that involve antibodies or molecule inhibitors which may provoke vascular damage. Effective strategies need to consider both the neurological and vascular outcomes of existing treatments.
Research surrounding TIM-3 and similar immune checkpoints could help illuminate pathways to mitigate these risks, potentially providing targeted solutions that address both brain and vascular health. By carefully designing therapies that focus on plaque removal without exacerbating vascular issues, there lies the potential for improved outcomes in patients experiencing both Alzheimer’s symptoms and vascular complications. This understanding further highlights the necessity of holistic treatment approaches in neurodegenerative diseases, emphasizing a balance between cognitive improvement and overall vascular integrity.
Future Directions in Alzheimer’s Research
As neuroscience continues to evolve, the future is bright for innovative Alzheimer’s therapies stemming from cutting-edge research on immune system dynamics and genetic factors. With ongoing studies focusing on TIM-3 and immunotherapy strategies, the horizon appears promising for treatments that could transform patient outcomes. Collaborative efforts across institutions and disciplines are crucial, fostering a multi-faceted approach that honors the complexity of Alzheimer’s disease. This cooperative paradigm promotes the development of therapies that could bridge the gap between basic research and clinical applications.
Moving forward, key areas of exploration will include determining the phases in which TIM-3-targeted therapies could be most beneficial, refining the use of anti-TIM-3 antibodies, and identifying optimal delivery mechanisms to the brain. As understanding grows around microglial functions and the intricate mechanisms of Alzheimer’s, the potential to reshape the therapeutic landscape increases. This integrated research effort holds promise not only for Alzheimer’s disease but may also have ripple effects in treating other neurodegenerative disorders rooted in similar biological pathways.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 checkpoint molecule to enhance the immune response of microglia, the brain’s immune cells. By blocking TIM-3, microglia are freed from inhibition, allowing them to clear amyloid plaques associated with Alzheimer’s, potentially leading to cognitive improvement in patients.
How does TIM-3 therapy relate to Alzheimer’s treatment?
TIM-3 therapy represents a novel approach in Alzheimer’s treatment that repurposes immune system strategies used in cancer therapy. By inhibiting TIM-3, researchers aim to enhance the clearance of harmful amyloid plaques in the brain, which could improve cognitive function in Alzheimer’s patients.
What role do microglia play in TIM-3 therapy for Alzheimer’s disease?
Microglia, the brain’s immune cells, are crucial in TIM-3 therapy for Alzheimer’s disease. The therapy aims to deactivate TIM-3, enabling microglia to attack and eliminate amyloid plaques in the brain, which could restore cognitive functions and help manage Alzheimer’s symptoms.
Can TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Yes, TIM-3 therapy has shown potential in improving cognitive function in mouse models of Alzheimer’s disease. By enhancing microglial activity and reducing plaque accumulation, it may lead to better memory and cognitive performance in affected individuals.
Is TIM-3 an immune system checkpoint relevant to Alzheimer’s disease?
Yes, TIM-3 is an immune system checkpoint molecule that can inhibit immune responses. In Alzheimer’s disease, high levels of TIM-3 on microglia prevent them from clearing amyloid plaques, contributing to disease progression. Targeting TIM-3 could help restore their function.
How could anti-TIM-3 antibodies be used in Alzheimer’s treatment?
Anti-TIM-3 antibodies could block the inhibitory effects of TIM-3 on microglia, enabling them to clear amyloid plaques more effectively. This approach could represent a significant advancement in Alzheimer’s treatment, leveraging existing cancer therapies for neurological benefit.
What are the implications of cancer treatment repurposing in TIM-3 therapy for Alzheimer’s disease?
Repurposing cancer treatments, particularly those targeting TIM-3, holds promise for Alzheimer’s disease by utilizing established mechanisms to enhance microglial function in the brain. This could lead to innovative therapies that effectively address cognitive decline in Alzheimer’s patients.
What is the significance of TIM-3 gene polymorphism in Alzheimer’s disease?
Polymorphisms in the TIM-3 gene are linked to late-onset Alzheimer’s disease and may affect the expression levels of TIM-3 on microglia. Understanding these genetic factors can guide personalized approaches in TIM-3 therapy for improved treatment outcomes.
What did studies on TIM-3 gene deletion reveal about Alzheimer’s treatment?
Studies using mice with TIM-3 gene deletion have demonstrated enhanced clearance of amyloid plaques and improved cognitive behaviors. These findings suggest that inhibiting TIM-3 in humans could provide a new therapeutic strategy for combating Alzheimer’s disease.
What are the next steps in developing TIM-3 therapy for Alzheimer’s disease?
Future research will focus on testing anti-TIM-3 antibodies in humanized animal models of Alzheimer’s disease to evaluate their effectiveness in halting plaque development and improving cognitive functions, paving the way for potential human trials.
| Key Point | Details |
|---|---|
| Research Background | A new strategy involving TIM-3, a checkpoint molecule, shows promise in targeting Alzheimer’s disease, similar to treatments used for some cancers. |
| Role of TIM-3 | TIM-3 inhibits microglia from clearing amyloid plaques, which are harmful accumulations in the brain associated with Alzheimer’s. |
| Importance of Microglia | Microglia are brain immune cells essential for cognitive function, but their activity is hindered by TIM-3, preventing them from clearing plaques. |
| Mouse Model Findings | Deleting TIM-3 genetically in mice improved cognitive function and reduced plaque burden significantly. |
| Potential Human Therapy | Future therapies may involve anti-TIM-3 antibodies or small molecules to block TIM-3’s activity, thereby enhancing plaque clearance. |
| Research Collaboration | The study involved collaboration between labs and utilized specific mouse models to further explore TIM-3’s role in Alzheimer’s. |
Summary
TIM-3 therapy for Alzheimer’s disease represents a promising novel approach in combating brain plaque accumulation and restoring memory function. By targeting the TIM-3 checkpoint molecule, researchers aim to enhance the immune response of microglia, the brain’s immune cells, to clear harmful plaques effectively. This innovative strategy not only highlights the potential for repurposing cancer therapies for neurodegenerative conditions but also marks a significant step forward after numerous setbacks in Alzheimer’s treatments. As the research progresses towards practical human applications, TIM-3 therapy could pave the way for new, efficacious treatments for Alzheimer’s, offering hope to millions affected by this devastating disease.